What is a Pressure Sore?
Did you know that more than 2.5 million people develop pressure sores (Bedsores) annually.
The Agency for Healthcare Research & Quality (AHRQ) estimates that more than 2.5 million people develop pressure sores (bedsores) annually. Pressure sores, also known as bedsores, pressure ulcers, or decubitus ulcers, are an injury to the skin and underlying tissue. They are caused by unrelieved pressure built up on an area of the skin for a long period.
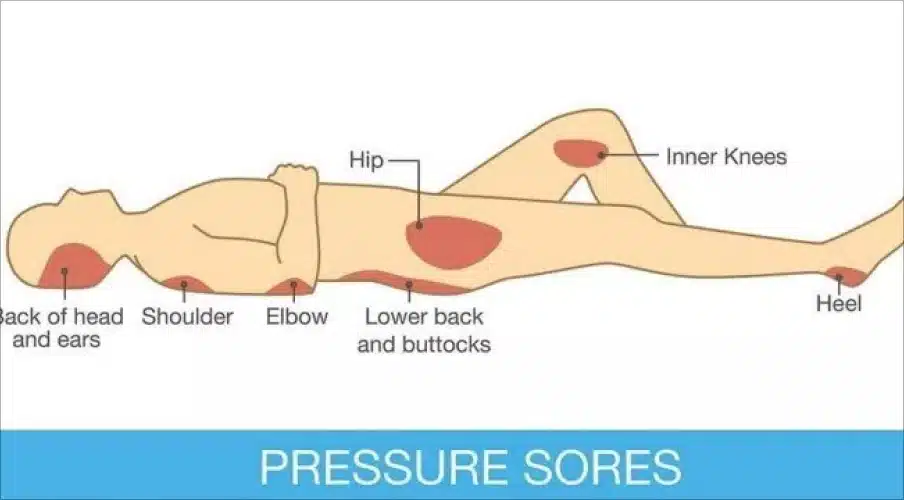
Pressure sores can range from mild reddening of the skin to severe tissue damage and sometimes infection that extends into muscle and bone. Pressure sores also known as bed sores, are often a sign of neglectful care at nursing homes, assisted living facilities, and hospitals. Due to the built-up pressure, blood flow to the affected area will become restricted, and the tissue may begin to die, usually starting with the skin. Pressure sores are most likely to develop in areas of the body with little to no muscle or fat for padding. These areas of the body are generally bonier and are more susceptible to the development of pressure sores. The most common places for pressure sores are the head, heels, back, and buttocks.
How Do Pressure Sores (Bedsores) Occur?
Bedsores or pressure sores can be painful and dangerous to our elderly who might not have the strength to get up and on their feet, or even reposition themselves in bed often enough to prevent the sores from happening.
Simply put, pressure sores occur when a person lays or sits in one position for a very long time. The pressure of the body causes all the blood to leave the area. The lack of blood flow causes tissue to die. The amount of time this takes will vary depending on the overall health of the person and the condition of their skin.
Pressure sores can occur in several ways. For example, after surgery or an injury, a person may be bedbound for a long time. Another example involves elderly people who cannot get out of bed or must use a wheelchair. Both examples commonly occur in nursing homes and assisted living facilities. Additional factors that put nursing home and assisted living facility residents at risk for developing bedsores include:
- Being elderly
- Needing assistance to move
- Malnourishment
- Incontinence
- Chronic health problems
- Fragile skin
- Alzheimer’s disease
- Dementia
What Are the Stages of a Pressure Sore (bedsore)?
The development of a bedsore (pressure sore) over time, and how to recognize them to prevent them from getting worse.
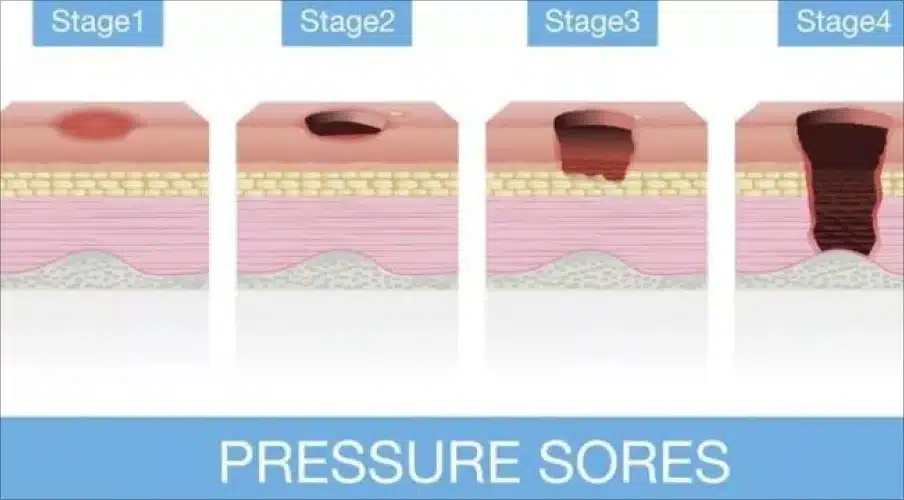
Pressure sores (bedsores) develop in four stages, with one being the least severe and four being the most severe. Each stage has different signs and treatment requirements:
Stage One: There are no open wounds or tearing. Instead, the skin appears red and may be painful to the touch. The pressure sore’s appearance may be very similar to a rash. When you press on the sore, the redness does not disappear. Skin temperature may be increased, and the skin may feel softer or firmer than the skin around it.
How to get rid of a Stage One sore: Take all pressure off the site of the wound. Keep the wound dry and clean. Make sure the patient’s diet is high in protein, Vitamin A, Vitamin C, zinc, and iron. Drink a lot of water to stay hydrated. Pressure sores at this stage can be reversed in about three days following proper care steps.
Stage Two: The skin is broken and begins to wear away or form an ulcer. The wound is likely to be tender and painful. The sore has reached the deeper layers of the skin but does not go all the way through the skin. At this stage, the wound may look like a scrape or blister filled with clear fluid. Some of the skin may be damaged beyond repair at this point.
How to get rid of a Stage Two sore: Follow the same steps as a Stage One pressure sore. The sore should go away within three weeks.
Stage Three: The sore will worsen and spread deeper to the tissue beneath the skin, although bone, muscle, or tendon will not be showing. Fat may be seen in the sore. Look for signs of infection like redness around the edges, pus, odor, fever, or a greenish discharge from the sore.
How to get rid of a Stage Three sore: Make sure all pressure is off the wound if this has not been done already. Go see a health care provider immediately. Pressure sores at this stage need special care from a medical professional. Healing time may be between one and four months.
Stage Four: The sore will be deep enough to cause damage to muscle, bones, tendons, and joints. There is a high risk of infections at this stage. Signs of infection are listed in the previous stage.
How to get rid of a Stage Four sore: Contact a health care provider immediately. Surgery is often required to treat such a severe pressure sore. Healing time can range from three months up to two years.
Are Pressure Sores (bedsores) Avoidable?
Stage One pressure sores and most Stage Two pressure sores may be unavoidable. However, with diligent care, the Stage One and Stage Two pressure sores are easily treatable. Furthermore, proper treatment should prevent them from becoming Stage Three or Stage Four pressure sores. As a result, most medical professionals agree that severe pressure sores, especially in stages three and four, are easily prevented.
In fact, developing a severe pressure sore in a nursing home is often a sign of nursing home neglect. Similarly, developing a severe pressure sore in an assisted living facility can be considered an indication of assisted living facility neglect.
How to Prevent the Development of Pressure Sores (bedsores)
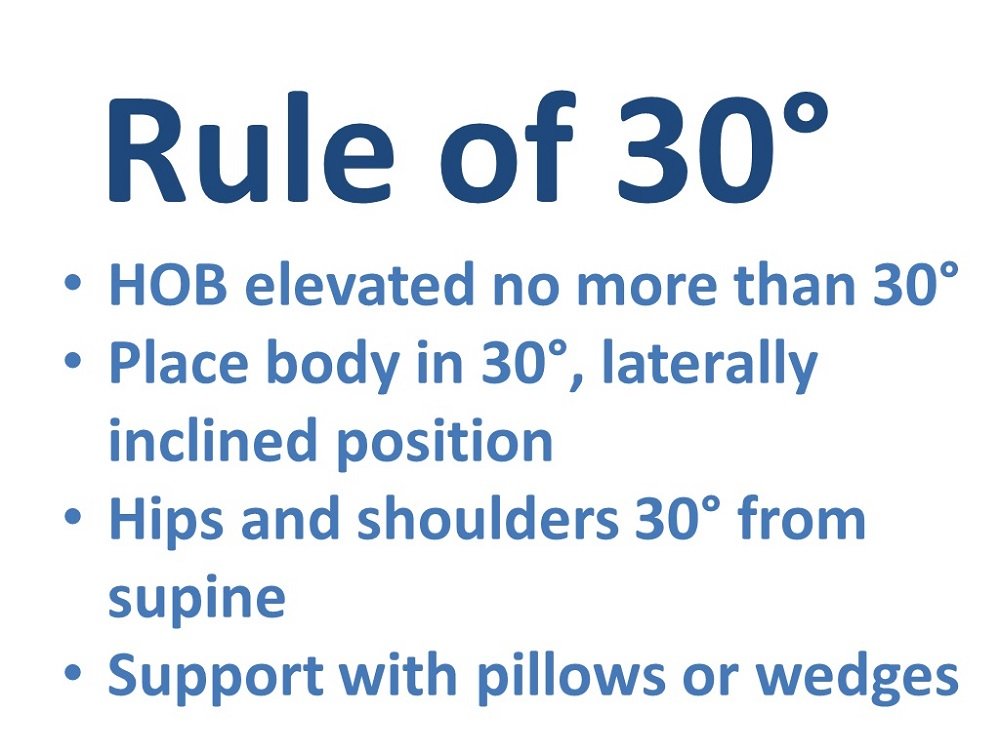
The most important intervention for the prevention of pressure sores is pressure relief. Standard pressure relieving techniques in nursing homes and assisted living facilities involve turning and repositioning bedbound and wheelchair-bound residents every two hours.
For someone who is bedbound, this means a staff member must help the person adjust in their bed from their left side to back to their right side every two hours. For someone in a wheelchair, this means assisting the person in repositioning in the wheelchair every two hours. It can also mean transferring the person out of a wheelchair into a bed or out of bed and into a recliner.
Other standard pressure-relieving techniques involve using pressure-relieving devices. For bedbound residents, this may mean a special pressure-relieving mattress. For wheelchair-bound residents, it may mean a special pressure-relieving pad in the wheelchair. For people at risk of developing heel pressure sores, it may mean floating the heels with pillows or using special pressure-relieving booties.
Preventing a pressure sore (bedsore) can be easy if you know what to look for.
Another important pressure sore intervention involves dealing with a person’s underlying medical conditions. For example, providing proper nutrition to malnourished individuals and providing proper hydration to dehydrated individuals gives the body the ability to help heal itself. Routinely cleaning people who are incontinent of bowel or bladder keeps the skin from breaking down and helps prevent skin irritations from becoming infected.
What Is the Number One Cause of Pressure Sores (bedsores) Developing in Long-Term Care Facilities?
The number one cause of pressure sores in nursing homes and assisted living facilities involves the staff not doing their job. Occasionally, the staff is not properly trained, or the staff is too lazy to do their job. However, most nursing home and ALF employees actually care about their residents and want to do a good job. The real culprit is the facility failing to provide enough staff.
Understaffing occurs when facilities cut down on the level of staff members to increase their profits. Understaffing also occurs when one caregiver is responsible for too many patients who have too many needs. In either situation, there is simply not enough time for the staff members to provide all the care that each resident needs. Turning and repositioning take time and, therefore, are often the first things an overworked staff member skips.
Who Is Responsible for Your Loved One’s Pressure Sores (bedsores)?
Responsibility for your loved one’s pressure sores will generally fall upon the facility where your loved one lives. Individual caregivers could also be liable.
You may generally sue a nursing home or assisted living facility if they are negligent. An attorney may prove negligence by:
- Showing the liable party owed your loved one a duty of care: Nursing homes and assisted living facilities, in most cases, owe their residents a duty of care. This duty of care requires the facility to take reasonable measures to prevent harm to your loved one, including pressure sores.
- Showing the liable party breached its duty of care: It’s a lawyer’s job to show exactly how a liable party breached its duty of care. In the case of pressure sores, the nursing home may have breached its duty by failing to hire enough staff or train its staff properly. Individual caregivers could be liable for simply failing to take measures to prevent pressure sores.
- Linking the liable party’s breach of duty of care to your loved one’s losses: An attorney will aim to prove that the liable party’s negligence caused your loved one’s damages.
- Showing the damages that resulted from the liable party’s negligence: A lawyer will show all the negative consequences, including pain and additional medical care, that resulted from the liable party’s negligence.
Different legal standards can apply to elder neglect cases. Your attorney will make appropriate arguments for liability based on the facts of your loved one’s case.
Recoverable Damages in an Elder Neglect Case
Your loved one may receive compensation for the damages they’ve suffered. While such damages will not undo the pain and suffering your loved one has endured, they are a way to instill justice for negligence. Recoverable damages may include:
- The cost of your loved one’s stay in the facility where they developed a pressure sore
- The cost of medical care for one or more pressure sores
- Their pain and suffering and any treatment they need for psychological and emotional trauma
- The cost to relocate your loved one to a new facility
- Any other damages stemming from neglectful care
An attorney will create an in-depth record of your loved one’s damages. They will pursue full compensation from the liable facility and any other liable parties.
Other Signs and Symptoms of Neglect in a Nursing Home or Assisted Living Facility
Pressure sores may be just the tip of the iceberg. You may look for other signs of neglect or abuse, which may include:
- Changes in your loved one’s personality
- Financial irregularities
- Other wounds in addition to the pressure sores
- Poor hygiene
- A disheveled personal appearance
- Unclean bedpans
- Indications that your loved one is in fear of their caregivers
If you see any reason for concern, then you must investigate further. Our Distasio Law Firm attorney and our team will help you identify any mistreatment that your loved one has suffered. Give us a call today for your free consultation, or submit a contact request form. We will review the legal options you have in pursuing compensation for your loved one’s pressure sores.
As an ethical and trusted personal injury lawyer, Scott Distasio founded Distasio Law Firm in February of 2006, which focuses on all types of personal injury cases. He wanted to open a law firm that represented his belief that all firms should provide ethical and outstanding service to their clients.



